
This article was originally featured on Knowable Magazine.
The patient’s teeth appeared to be well cared for, but dentist James Mancini did not like the look of his gums. By chance, Mancini knew the man’s physician, so he raised an alert about a potential problem—and a diagnosis soon emerged.
“Actually, Bob had leukemia,” says Mancini, clinical director of the Meadville Dental Center in Pennsylvania. Though he wasn’t tired or having other symptoms, “his mouth was a disaster,” Mancini says. “Once his physician saw that, they were able to get him treated right away.”
Oral health is tightly connected to whole-body health, so Mancini’s hunch is not surprising. What is unusual is that the dentist and doctor communicated.
Historically, dentistry and medicine have operated as parallel fields: Dentists take care of the mouth, physicians the rest of the body. That is starting to change as many initiatives across the United States and other countries work to integrate oral and whole-body care to more effectively tackle diabetes, cardiovascular disease, joint replacements and many other conditions. The exact relationship between health of mouth and teeth and physical ailments elsewhere in the body is not well understood—and in some cases, is contentious—but experts agree there are links that should no longer be overlooked.
In recent years, dental hygienists have started working in medical clinics; physicians and dentists have started a professional association to promote working together; and a new kind of clinic—with dentists and doctors under one roof — is emerging.
“We are at a pivotal point—I call it the convergence era—where dentistry is not going to be separated from overall health for much longer,” says Stephen E. Thorne IV, founder and CEO of Pacific Dental Services, based in Irvine, California. “Dentistry will be brought into the primary care health-care team.”
Sick mouth, sick body
The list of connections between oral health and systemic health—conditions that affect the entire body—is remarkable. For starters, three common dental issues—cavities, tooth loss and periodontal disease—are all associated with heart disease, the leading cause of death in the United States. “To me, the number one hidden risk factor for the number one killer in our country is oral health,” says Ellie Campbell, a family physician in Cumming, Georgia, and board member of the American Academy for Oral Systemic Health, founded in 2010 to increase awareness of how oral and whole-body health are related.
Periodontal disease, infection and inflammation of the gums and bone that support the teeth, is the main culprit. Nearly half of adults 30 and older have periodontal disease; by age 65, the rate climbs to about 70 percent. In the early stages, called gingivitis, gums are swollen and may bleed. Periodontitis, a more serious condition in which gums can pull away from the teeth, is the sixth most common human disease.
Periodontitis is associated with a slew of systemic ills: heart attacks, strokes, heart failure, diabetes, endocarditis, chronic kidney disease, recurrent pneumonia, chronic obstructive pulmonary disease, gastritis, rheumatoid arthritis, cancer and cognitive impairment.
Bad habits, including tobacco use, alcohol consumption and high-sugar diets, are implicated too. They raise the risk for cavities and most oral diseases, and are also linked to ills such as cancer, chronic respiratory disease and diabetes.

Such connections were apparently lost on officials at the University of Maryland in 1837, when the university rebuffed a proposal from two physicians to teach dentistry to the school’s medical students. At the time, medicine wanted nothing to do with dentistry, which was practiced by unregulated and inadequately trained itinerants, says medical and dental historian Andrew I. Spielman, a dentist and oral surgeon at the New York University College of Dentistry. “There were a lot of charlatans,” he says. “They had a very bad reputation.”
The dismissal prompted the rejected physicians, Horace Hayden and Chapin Harris, to establish the world’s first dental school, the Baltimore College of Dental Surgery. Today, dentistry is a highly regulated profession, and the United States has 73 accredited dental schools.
Despite their disparate training, both doctors and dentists are aware that mouth health is important to whole-body health, Campbell says. “Ask a family practice doctor and they will say ‘Oh yeah, if the patient has diabetes, they’re going to have bad teeth and gums, and I can never get their diabetes better until the dentist fixes their gums,’” she says. “And the dentist is going to say, ‘Well, I’ll never get their gums better until the primary care doctor gets their sugar under control.’”
Mancini, the Pennsylvania dentist, says dentists often are asked to examine a patient’s mouth before physicians will proceed with certain treatments. “Physicians know any infection in a patient who’s being treated for cancer could be very much life-threatening,” he says. “The orthopedic guys are now sending all of their patients to the dentist for the same reason.”
Hurdles to holistic care
But working together to improve a patient’s health is not as simple as it might seem. A decade ago, the federal government hired the National Network for Oral Health Access to run a pilot program merging oral and primary health-care centers. The network’s dental consultant, Irene Hilton, a dentist with the San Francisco Department of Public Health, said three barriers to integration became clear.
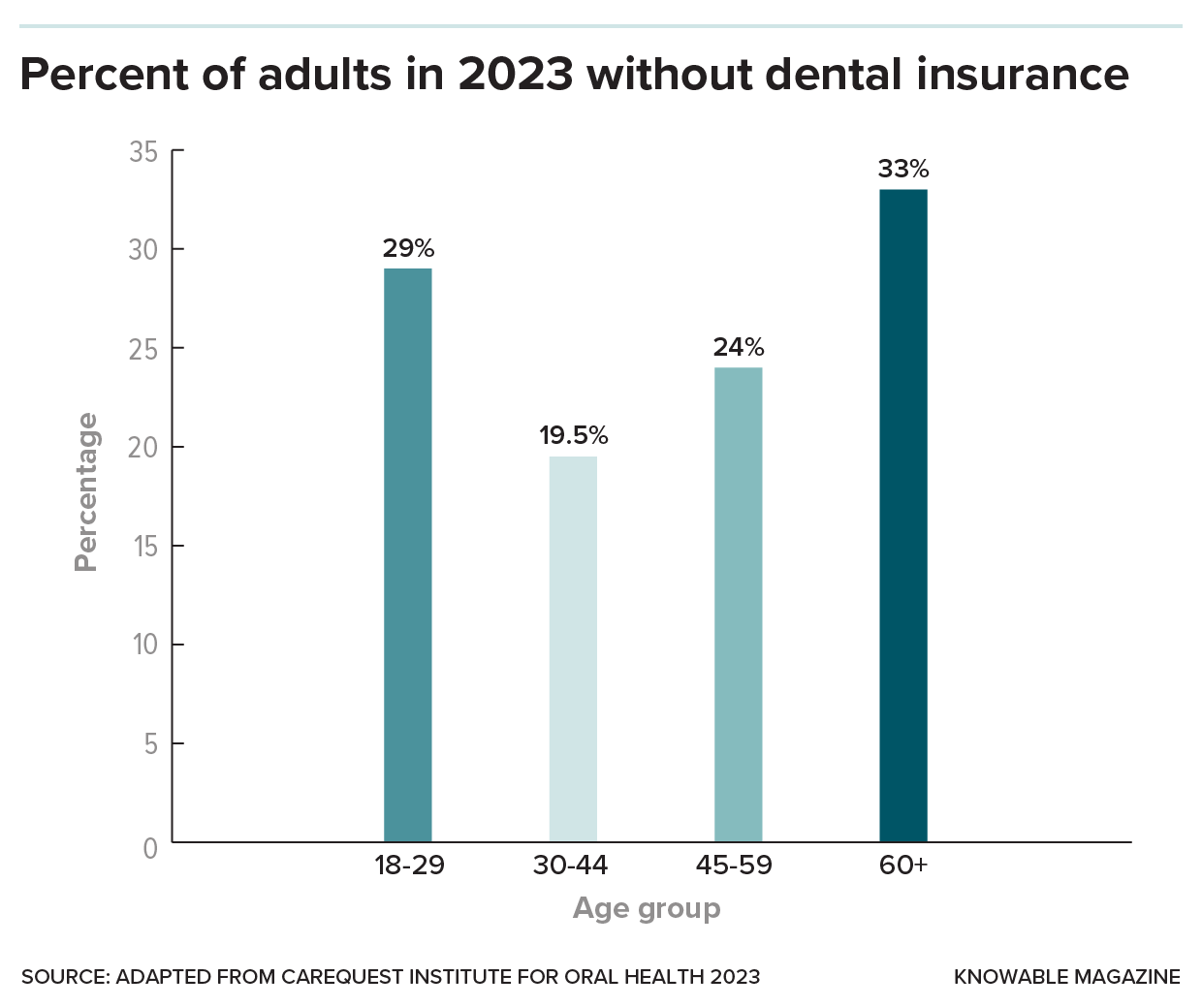
The fragmented way that health care and dental care are paid for is one of them. While more than 90 percent of Americans have health insurance, only 77 percent of US adults ages 19 to 64 have dental coverage, which typically is sold separately from health insurance. The nation’s largest insurer—the federal Medicare program—generally does not cover dental services, and nearly half of Americans 65 and over have no dental coverage.
That causes problems for patients who need, say, a joint replacement that would be covered by insurance but who cannot afford the dental work that is needed in advance. Surgeons won’t replace a knee until patients first get their dental work done, Mancini says, “so we’re kind of the barrier to them improving their life.”
Another barrier is that dentists and physicians are not routinely trained to work with each other, Hilton says.
Dental students study anatomy, physiology and other sciences related to the whole body, then home in on clinical care for mouth and teeth. But many physicians have almost no training in oral health. A 2009 survey found that 10 percent of medical schools that responded offered no oral health curriculum, and 69 percent offered fewer than five hours on the subject.
A third issue is what Hilton calls infrastructure. In most cases, the electronic health records used by physicians are incompatible with those used by dentists, so sharing information electronically is impossible. Likewise, dental offices are typically not embedded in medical clinics, where doctor-dentist referrals might be easier.
If oral and systemic health are to be integrated broadly, “these are the things that have to be overcome or addressed,” Hilton says.
The situation is not much different in other parts of the world. In 2021 the World Health Organization—noting that oral diseases are a global public health problem affecting nearly 3.5 billion people—recommended that dentistry focus more on prevention and be more integrated with primary care services.
Demonstrated links
In the past quarter-century, a great deal of research has demonstrated the links between oral and whole-body health. For example, when researchers followed 15,456 patients from 39 countries with stable coronary heart disease for nearly four years, they found that those who had lost the most teeth had the highest risk of having a stroke, heart attack or cardiovascular death. Similarly, a study that tracked 7,466 US adults ages 44 to 66 for an average of 14.7 years revealed that those who had severe periodontitis had a greater risk of cancer than those with no or mild periodontitis.
In 2015, the Harvard School of Dental Medicine launched an initiative to support integration of the two fields—in education, insurance and professional practice. (The initiative gets funding from dental product brands and health insurance companies, and Thorne, the Pacific Dental Services CEO, serves on its board.) “We’ve published papers identifying links between periodontal disease and diabetes, hypertension, dementia, adverse birth outcomes, low birth-weight babies, preterm birth, spontaneous abortion, kidney disease,” says Jane Barrow, the initiative’s executive director.
But correlation is not the same as cause and effect, and scientists have not nailed down the exact relationship between periodontitis, which affects more than 11 percent of the global population, and various systemic diseases.
Periodontitis is associated with bacteria in the bloodstream and systemic inflammation, which can affect organs such as the liver and bone marrow. That, in turn, can trigger or aggravate other conditions. And the periodontal bacteria—that travel via the bloodstream, inhalation or ingestion—may also cause infections or exacerbate inflammation in other parts of the body.
When the major professional societies for periodontology in the United States and Europe convened a group of global experts in 2012 to review the science, they concluded that it was “biologically plausible” that the inflammation of periodontitis ups the risk of cardiovascular disease and influences type 2 diabetes and other maladies – but “plausible” was as far as they would go.
Seven years later, the European Federation of Periodontology and the World Heart Federation again gathered experts to review new studies on the link between periodontitis and cardiovascular problems. Again, though scientists had made some headway in identifying possible biological mechanisms to explain the link, experts have since concluded that the evidence does not yet prove that periodontitis actually causes strokes, heart attacks or anything else.
Flipping the question on its head, does preventing or treating periodontal disease help to prevent heart problems? Several observational studies, in which researchers observe individuals and measure particular outcomes, but don’t intervene, suggest that oral health care, including toothbrushing and dental cleanings, make a difference. For example, a study that tracked the health habits of 11,869 adults 35 and older in Scotland found that within eight years, those who rarely brushed their teeth had more cardiovascular problems compared with those who brushed twice a day.

That still does not prove that preventing periodontitis will hold heart problems at bay: Some other habit or feature of the toothbrushing group could have been the important factor. The relationship is difficult to tease out, Barrow says, because people who are taking good care of their mouths tend to take good care of themselves in general. “Could you say that people who are taking care of their mouths are in better health overall? You would probably find that to be true,” she says. “Is it because they’re taking care of their mouth? I can’t say that.”
And nobody else should say that either, according to a 2018 editorial in the Journal of the American Dental Association. The coauthors, a group of dental and public health researchers, cautioned against overstating the oral-systemic health connection. “The main reason for maintaining good oral health is because it is important in and of itself,” they wrote.
One of the contributors, Bryan Michalowicz, a dental researcher at HealthPartners Institute in Minnesota, later led a team that reviewed the medical records and insurance claims of 9,503 patients to see if periodontitis treatment improved the health outcomes of those with coronary artery disease, cerebrovascular disease or type 2 diabetes.
Overall, cardiovascular patients who received dental treatment and follow-up maintenance saw no difference in the rate of heart attacks, strokes, bypass surgeries or angioplasty procedures compared to those who were not treated, the team reported in 2023. Likewise, periodontal treatment did not significantly lower the blood-sugar levels in patients with type 2 diabetes.
Overdue integration
But the data suggesting connections have been enough to spark many grassroots efforts at integration. In addition to the American Academy for Oral Systemic Health, the National Network of Healthcare Hygienists, founded by hygienist Jamie Dooley in 2018, helps prepare hygienists who want to integrate oral health into health-care systems.
And in California, Thorne’s business is trying to make those interactions easy by putting dental and medical services under one roof. In December 2023, Pacific Dental Services opened a clinic, Culver Smiles Dentistry, in a space shared with a medical practice. It’s the first of 25 planned dental-medical practices that will operate through a partnership between MemorialCare, a big Southern California health system, and Pacific Dental.
Health-care leaders, Thorne says, are beginning to realize that they can improve their patients’ health by incorporating dental care into primary care.
It’s sort of crazy, he says, that our mouth and our jaw and our throat have been considered separate from the rest of our body for so long. “It is changing now, and health care is realizing that the mouth is the gateway to so much of our overall health.”
This article originally appeared in Knowable Magazine, an independent journalistic endeavor from Annual Reviews. Sign up for the newsletter.
The post Why isn’t dental health considered primary medical care? appeared first on Popular Science.
Articles may contain affiliate links which enable us to share in the revenue of any purchases made.
from Popular Science https://ift.tt/u2wsQdZ




0 Comments